Introducing your baby to solid foods is an exciting time, but one common question is, “When can babies eat salt?” It’s essential to understand the appropriate age and risks associated with salt consumption for babies.
In this article, we’ll delve into the topic and provide you with valuable insights on:
- Risks of excessive salt consumption for babies
- Recommended sodium levels for infants
- Average sodium content in breast milk and formula
- High-sodium foods to avoid for babies
- The impact of adding salt to baby food on their future taste preferences
- Best alternatives to using salt
Read on to learn more about when it’s safe to introduce salt to your baby’s diet and how to ensure their health and well-being during this crucial stage of development.
Key Takeaways
- Consuming too much salt during infancy and childhood can cause health problems like high blood pressure, kidney damage, and a lifelong preference for salty, ultra-processed foods.
- Recommended sodium levels for infants are 110mg daily for babies under 6 months and 370mg daily for babies aged 7-12 months. Breast milk and formula already contain sodium.
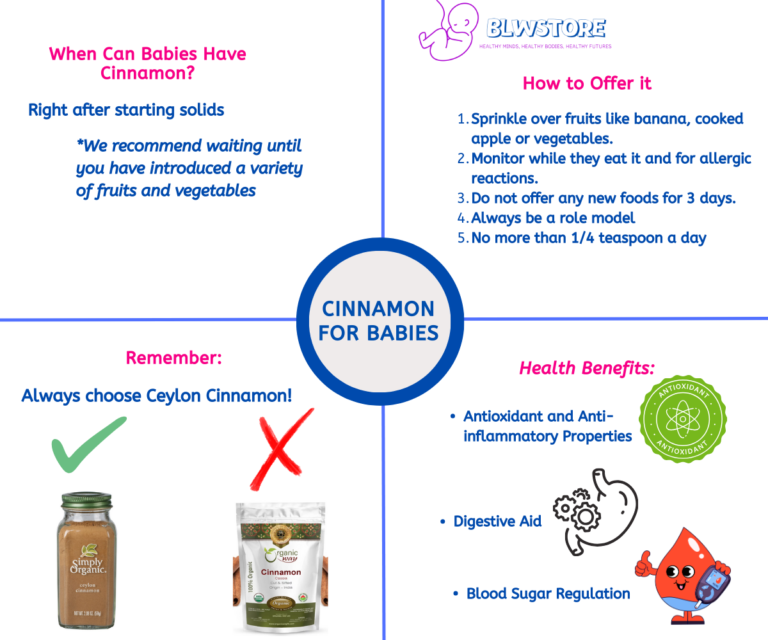
- Adding salt to baby food is unnecessary and not supported by safety research. Instead, consider using spices to introduce new flavors.
- Processed foods high in sodium should be avoided for babies, and healthier, low-sodium options should be introduced.
- Research on whether adding salt to baby food causes a preference for salty foods later in life is inconclusive, but it is still best to avoid adding salt during the first 24 months.
Watch it in Youtube!
What are the risks of consuming too much salt for babies?
You may want to add salt to your baby’s food hoping that it’ll improve the taste and encourage your baby to eat.
Perhaps, you are doing baby-led-weaning and you want to serve your baby the saltier foods you cook for you or the rest of the family. However, giving your baby too much salt over time may cause health problems, such as high blood pressure. In extreme and rare cases, a baby that’s had a large amount of salt may even end up in the emergency room.
Too much salt during infancy and childhood may also promote a lifelong preference for salty foods and ultra-processed, which are a danger to our health.
A baby’s kidneys are still immature, and they aren’t able to filter out excess salt as efficiently as adult kidneys. As a result, a diet that’s too rich in salt may damage a baby’s kidneys. A salt-rich diet may also affect a baby’s long-term health and taste preferences.
Repeatedly being offered salty foods may reinforce babies’ natural taste preference for salty and sweet foods, possibly causing your child to prefer salty foods over those that are naturally less salty, such as vegetables.
As a result, babies fed a salt-rich diet tend to have higher blood pressure levels during childhood and adolescence, which may increase their risk of heart disease later in life.
Too much salt during infancy and childhood may cause health problems, such as high blood pressure and kidney damage, and promote a lifelong preference for salty and ultra-processed foods, increasing the risk of heart disease later in life.
What are the recommended sodium levels for infants?
The amount of sodium that your baby needs daily is determined by their age. Infants who are 6 months and under should consume 110 milligrams of sodium, while babies aged 7 to 12 months should have a daily intake of 370 milligrams.
Keep in mind that breast milk and formula also have sodium in them and they cover every need your baby has for the first 6 months.
When it comes to feeding babies and toddlers, adding salt to their meals is totally unnecessary and not backed by any kind of safety research.
If your little one is eyeing something salted that you are having, think about how it was cooked. Is it a frozen, ready-made, canned or takeout food item?
It may be better to just not give that portion or even skip it. For homemade meals where a bit of salt was used, it should be alright.
However, if you often share food with your baby, it is worth cutting down on your own salt consumption.
What is the average sodium content of breast milk and formula?
The salt content between breast milk and formula can differ depending on the source; usually, breast milk contains 6-12 mg of sodium for every 100ml, while formula has an average of 40 mg of sodium per 100ml.
Breast milk has naturally less salt than formula, but this could vary due to the mother’s diet and the type of formula being used.
Are there any foods that are especially high in sodium that should be avoided for babies?
Meats and Seafood:
- Processed meats (salami): 1,740 mg/100g
- Deli meats: 1,300 mg/100g
- Anchovies: 3,600 mg/100g
- Cured fish (herring): 250 mg/100g
Prepared Foods and Meals:
- Canned soups and broths: 800 mg/cup
- Prepared frozen meals: 700-1,000 mg/100g
- Instant noodles: 860 mg/100g
- Fast food burgers and fries: 440 mg/100g
- Pizza: 600 mg/100g
Snacks and Crackers:
- Packaged snacks (chips, popcorn): 300-500 mg/100g
- Salted nuts: 317 mg/100g
- Crackers: 750 mg/100g
Condiments, Sauces, and Dressings:
- Pickles and olives: 1,200 mg/100g
- Soy sauce: 5,500 mg/100g
- Ketchup, mustard, BBQ sauce: 900 mg/100g
- Gravies and sauces: 430 mg/100g
- Salad dressings: 830 mg/100g
Dairy and Baking:
- Cheese: ~800 mg/100g (depends on type) *Do not offer cow’s or goat’s milk before the 12-month mark
- Regular baking mixes: 1,500 mg/tablespoon
- Instant oatmeal: 50 mg/100g
Keep in mind that processed foods have high salt content and should not be offered to babies. Introduce healthier, low-sodium options instead.
Will adding salt to baby food cause them to prefer salty foods later in life?
Research has not yet reached a definitive answer regarding whether adding salt to baby food will cause them to prefer salty foods later in life.
Some research suggests that the addition of salt to baby food may increase the preference for salty flavors in older children and adults, however, other studies have failed to find an association between early salt exposure and salt preference later in life.
Additionally, adding any type of seasoning to baby food may help introduce new flavors that could be beneficial to developing taste preferences, however this seasoning should be with natural spices and nothing processed or artificial.
Adding salt to baby food may increase the preference for salty flavors in older children and adults, but research has not yet reached a definitive answer.
What is the best alternative to using Salt?

Babies under 6 months of age meet their daily sodium requirements from breast milk and formula alone.
7–24-months-old are able to meet their needs from breast milk or formula and the small amounts of sodium naturally present in unprocessed complementary foods.
As such, experts recommend that you don’t add salt to your baby’s food during their first 24 months.
Having an occasional meal with salt added is OK. You may sometimes feed your baby some processed foods with salt added or let them try a meal from your plate. That said, overall, try not to add salt to the foods you prepare for your baby.
After the age of 2, recommendations vary a little in Europe and the United States. However, the idea is the same: you can start to add some salt to your baby’s meals so you can all eat the same, but this amount should be no more than a teaspoon at the end of the day.
Nevertheless, let’s not forget that there are other ways to make your food tastier. Spices are a GREAT option to make your meals delicious. Just remember that you have to treat each spice as a new food and you should be introducing them first one at a time. Once you have introduced a few, you can use them together and try new combinations for your baby to experiment and taste new flavors.
Experts recommend not adding salt to your baby’s food during their first 24 months; instead, consider using spices to introduce new flavors and make meals delicious.
We’re Maria and Alberto, a married couple and educators who are nutrition enthusiasts. Even before we had kids, we were already crazy about nutrition.
We’d read scientific articles, watch videos from nutritionists, and spend hours listening to nutrition podcasts.
Today, we continue doing this, but in a different way, as we’ve learned to sift through the noise and trends. Nutrition, like any other field of knowledge, the more you read and learn, the more you develop a comprehensive understanding of reality, and that’s what has happened to us.
Before having our first child, we focused on learning everything we could about child nutrition, using the same techniques we had already employed, backed by our extensive knowledge in nutrition.
Our mission is to help other parents with their children’s nutrition, to help them become the best versions of themselves.
If we are what we eat and drink, which is absolutely true, let’s do it right!